
African Health Correspondent, BBC News
 Mike Elvis Tusubira
Mike Elvis TusubiraLife of motorcycle taxi rider Mike Elvis Tusubira has been turned upside down since U.S. President Donald Trump stopped foreign aid last month.
Not only is the 35-year-old worried about his survival because he took lifesaving antiretroviral (ARV) drugs — but he said he will have to break up with his wife because they can no longer make safe sex Behavior.
His partner is the head of HIV and relies on Prep, a drug that reduces the risk of HIV infection.
“It means my marriage will end, too, because there are no precautions in fact, she won’t stay.”
“No condoms, no (anti-HIV) lubricants, no preparation, nothing. We can’t live without meeting. It means I have to stay single.”
All of the couple’s drugs and birth control pills are attributed to funding from USAID, the major overseas aid agency of the U.S. government.
They have been unable to replenish their supplies since what he heard on social media about a sudden closure. His wife is now completely out of preparation and they both worry about relying on condoms alone – the remaining condoms – too risky.
Trump ordered a 90-day pause to foreign aid on his first day in office and has since begun issuing a stop order to the United States Agency for International Development-funded organizations.
The exemption was followed by a humanitarian project, but by then, the HIV program, Mr. Tasubila, was part of the Marpi Clinic in northern Kampala – Kampala (Kampala) had been closed.
He called his counselor at the city’s Kiswa Health Center III to find out what was going on.
“My consultant is in the village. He told me he is no longer in the clinic.”
A person’s father tested positive for HIV in 2022 and has since missed a test that could not determine how much virus and the strength of the immune system are in his blood.
“I’m moving in the dark. I don’t know if my viral load is suppressed. I’m traumatized.”
He believes that the job of driving a motorcycle taxi – locally known as “Boda -Boda” – will be able to help his family overcome the obstacles they are facing now.
“Others say these drugs will be in private pharmacies…As Boda-Boda rider, I don’t know if I can raise funds to maintain my treatment.”
He said they were also affected by losses in services provided by non-governmental organizations (NGOs) funded by the United States Agency for International Development.
His wife is getting preparations through Marpi’s NGO, while his five-year-old son is benefiting from his son who provides schools and food for vulnerable children.
“My kids are no longer in school,” he said.
 Getty Images
Getty ImagesUganda’s health sector relies heavily on donor funds that support 70% of its AIDS program.
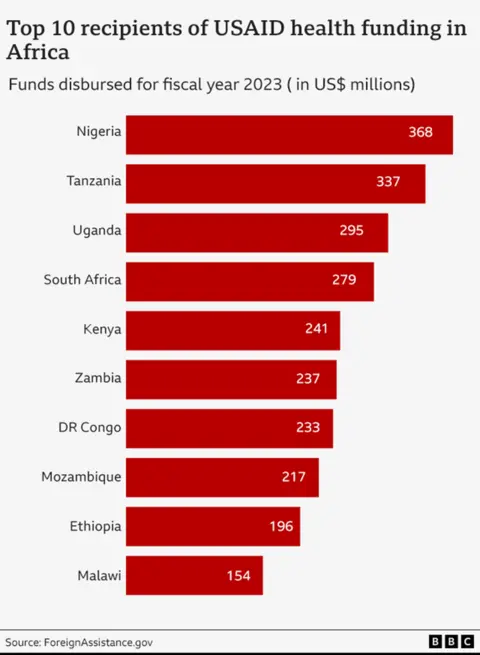
East African countries are one of the top ten recipients of the United States Agency for International Development Fund in Africa. According to the U.S. government, the country received $295 million (£234 million) in health financing from the agency in 2023 – third behind Nigeria, which received $368 million and $337 million from Tanzania.
USAID also supports its malaria, tuberculosis and leprosy programs – as well as funding maternal and child health services and emergency health assistance.
The U.S. funding freeze has been affected by thousands of healthcare workers.
Dr. Shamirah Nakitto, clinician with Mbuya (ROM), is a faith-based community organization that provides medical and psychosocial support for HIV patients in Uganda – based in Kisenyi Health Center IV, which provides population in Kampala Dense slums.
On average, she received 200 HIV/AIDS and tuberculosis patients a day. But after the order was stopped, all ROM-backed health workers were fired.
Now its TB unit remains silent, and its orphan and vulnerable children sector has also been closed in Kisenyi.
She told the BBC: “We are waiting for 90 days.
“It’s so sudden. We didn’t have a proper exchange on the facility. We just stopped working.”
Uganda’s Ministry of Health said it is exploring ways to minimize interference.
Diana Atwine, the Ministry’s top civil servant, urged staff to “will continue to work as volunteers”.

In southern Malawi, U.S.A.-IDP-funded activities have also ceased.
The country received $154 million in revenue from the United States Agency for International Development (USAID) health budget in 2023, making it the top ten recipient in Africa.
In the northern city of Mzuzu, the gates were closed in the clinic, which has been the main provider of HIV services in the region. Vehicles are idle; the Macro Mzuzu clinic shows no signs of activity. The worker locked the door, turned off the lights, and went home 18 days ago.
Although the U.S. State Department exemption on January 28 allows medical treatment (such as ARV), many clinics have been closed because there are no key personnel who coordinate USAID activities and distributing drugs is a challenge.
Even where service is technically allowed, many contracts are still in a dilemma. Health workers are not sure what they can and cannot do.
The Trump administration plans to reduce USAID staff by more than 90%.
Atul Gawande, former global health assistant administrator at the United States Agency for International Development (USAID), released on X that the agency’s workforce will be cut from 14,000 to 294, with only 12 employees allocated to Africa.
More than 30 NGOs in Malawi have also been severely affected by the funding freeze.
Eddah Simfukwe Banda, a 32-year-old survival farmer, has obtained ARV from Macro Clinic since 2017, where various NGOs offer HIV programs.
She fears her fate – and her sister son, who also relies on donor-funded drugs – and says they have no choice but pray.
She told the BBC: “We must pray like the Malawians. Those of us who believe in the God who relies on open the door when the door is closed.”
The mother of three children has three weeks left for ARV and also said that systemic failure is the culprit: “As Malawians, we are too dependent on assistance. Sometimes we are lazy and waste us.
“Let it be a lesson we have to be independent,” she said.
But this is difficult for one of the poorest and most dependent countries in the world. According to the World Bank, Malawi is vulnerable to external shocks – including prolonged droughts, cyclones and unstable rainfall.
In its healthcare system, this size of disruption presents a huge challenge.
For decades, the United States has been Africa’s most important public health partner.
In particular, through its groundbreaking plans to deal with the global spread of HIV launched in 2003. Called the U.S. Presidential AIDS Relief Emergency Plan (PEPFAR), it saved more than 25 million lives.
According to the African Centers for Disease Control and Prevention (Africa CDC), U.S. Agency for International Development has provided $8 billion in aid to Africa over the past year.
Jean Kaseya told BBC Newsday last month: “Seventy-three percent of people go to health care.”
Health experts warn that replacing the fund will be very difficult.
The African government has made great progress in reducing its dependence on aid. Kenya now provides funding for nearly 60% of its HIV response. South Africa covers nearly 80%.
But for many low-income countries, debt burdens, climate disasters and economic shocks make almost self-sufficient.
Amref Health Africa, one of the continent’s leading health NGOs, warned that global health security could be threatened without emergency action.
Its CEO Githinji Gitahi told the BBC: “This will require African governments and the African CDC to increase their own funds, which is under current debt-troubled conditions. It’s almost impossible.”
“With climate change and the accelerated outbreak of conflicts in human environment, this will make the world vulnerable and insecure – not only for Africa, but for everyone.”

Globally, there were 630,000 AIDS-related deaths and 1.5 million new infections in 2023.
Although infection rates have been declining in the worst-affected countries, the impact of the U.S.A.I.D. closures may reverse these gains.
“If you cancel this significant contribution from the U.S. government, we expect another 6.3 million AIDS-related deaths in the next five years,” Winnie Byanyima, head of UNAIDS, Tell the BBC’s daily podcast in Africa This week.
“There will be 8.7 million new infections, and 3.4 million AIDS orphans. I don’t want to sound like a doom prophet, but it’s my responsibility to give the facts as we see.”
Medical charity Sansantières (MSF) also warned of the danger of interrupting HIV treatment.
“Hidden daily use of HIV drugs or people are at risk of developing resistance or fatal health complications,” Tom Ellman, who is from Southern Africa, said in a statement.
Back in Uganda, Mr. Tusubila felt bleak about the future.
He has 30 days left with ARV medication – may choose to leave Kampala and go home after that.
“At least it would be easier. If I die, they just bury me there, not bothering me in Kampala.
“I can’t live here without ARV services.”
You may also be right:
 Getty Images/BBC
Getty Images/BBC




